
One of the most critical decisions in oncology drug discovery happens well before clinical trials begin: selecting the most impactful preclinical model.
Why? Because even the most promising therapies can still fail if the model used doesn’t accurately reflect the disease biology. That’s why it’s essential to consider model choice not as a box to tick, but as a strategic step that can determine the success of a program.
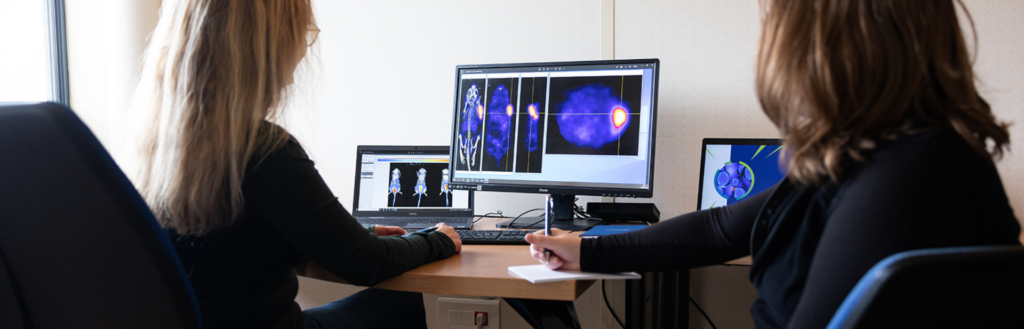
Thinking about Standard of Care First
Beyond the choice of model type and implantation site, which we’ll come to in a moment, it’s essential to remember how new therapies are actually used in the clinic. Physicians will almost always prescribe the current standard of care (SoC) first, whether it’s chemotherapy, targeted therapy, or immunotherapy. New drugs typically come into play for patients who relapse or fail to respond.
For drug developers, this means preclinical studies need to go further than testing a compound in isolation. The real questions are:
- Does my therapy add value compared to the current SoC?
- Can it be combined with SoC to improve outcomes?
Designing studies that incorporate SoC arms, whether as comparators or in combination, is critical to generating data that resonates with clinicians and regulators.
The Importance of Model Diversity
There is no “one-size-fits-all” model. The right choice depends on your therapeutic mechanism, disease indication, and stage of development. For this reason, it’s important to maintain a broad awareness of models, including:
- Syngeneic models for studying tumor–immune system interactions.
- CDX (cell line–derived xenografts) for reproducibility and robust efficacy testing.
- PDX (patient-derived xenografts) to capture tumor heterogeneity and clinical relevance.
Each of these model categories brings unique advantages and limitations. For example, syngeneic models are valuable for immunotherapy research but are limited by their murine immune background, while PDX models offer high translational value but can be resource intensive.
Why Implantation Site Matters
Beyond model type, the implantation site influences how tumors grow and behave:
- Subcutaneous models are easy to set up, reproducible, and allow direct monitoring, making them ideal for screening or comparing compounds.
- Orthotopic models recreate the tumor’s native environment, preserving local interactions and metastatic patterns. This is crucial when investigating tumor biology or microenvironement-driven responses.
Model selection is not a checklist exercise. It’s a strategic choice that needs to align with biology, clinical practice, and ultimately patient care. By considering diversity of models, implantation site, and how therapies will be positioned against standard of care, researchers can generate preclinical data that is not only rigorous but also truly translatable.