
Rethinking Brain Metastasis Models: A Step Closer to Clinical Reality
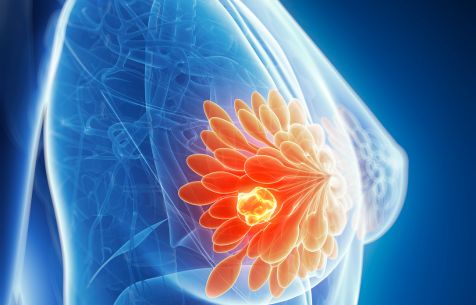
Brain metastases remain one of the toughest challenges in oncology. For patients with triple-negative breast cancer (TNBC) is usually identified at an advanced stage of cancer progression and the risk of developing metastases in the brain, bone, lung, or liver is high, and current treatment options remain limited. These metastases are often the cause of mortality, and yet, developing therapies that can effectively reach and treat them is still a major challenge.
One reason for this gap? The preclinical models we use to test potential therapies often don’t fully mimic the clinical situation.
The Challenge with Existing Models
Commonly, brain metastasis studies rely on stereotaxic injection, where tumor cells are placed directly into the brain. While this approach is technically straightforward and ensures tumor growth, it skips critical steps of metastasis: circulation in the blood, crossing the blood–brain barrier, and colonization in different brain regions. In other words, by stereotaxic injection, models don’t tell the full story.
For drug developers, this limitation can make it difficult to predict how a therapy will perform in real-world conditions.
A New Way Forward
To better align preclinical findings with clinical reality, our scientists turned to the intracarotid route. This strategy allows tumor cells to spread via the bloodstream, offering a model that preserves key biological steps and mirrors how metastases emerge in patients.
This innovative approach led to several important outcomes:
• Clinically relevant progression: Brain metastases developed in multiple regions, not just at one injection site.
• Better preservation of the blood–brain barrier: Unlike stereotaxic injection, oedema was reduced and barrier integrity maintained longer.
• Extended survival: Animals injected via the intracarotid route survived longer, providing a broader window to evaluate therapeutic effects.
Why This Matters
For researchers and drug developers, this means access to a more predictive and translatable model for testing new therapies against TNBC brain metastases. By reflecting the true clinical biology of metastasis, the model offers a stronger foundation for developing treatments that can genuinely improve patient outcomes.
By challenging the status quo in preclinical modeling, we’re not just running studies, we’re building bridges between early research and real patient needs.
This model was first presented at the AACR annual meeting in April 2025. You can read the details in the poster here.