Preclinical CRO Services for Inflammation of the Kidney
Acute and chronic inflammatory diseases of the kidney can be triggered by several causes of tissue injury such as exposure to toxins, auto-immune conditions or infections. Rodent models of kidney inflammation and injury are helpful to decipher disease triggering or sustaining mechanisms observed in patients.
Oncodesign Services offers CRO services for several preclinical models addressing a variety of kidney diseases, and provides CRO support to the de novo development of new kidney inflammation models recently described in literature.
Typical readouts for kidney inflammation models
- Clinical scoring
- Body weight
- Histopathology
- Biomarker/drug monitoring
- Gene expression in kidneys, by qPCR/dPCR
Kidney Inflammation Models List
Oncodesign Services offers kidney models as :
- Acute kidney injury model in mice, induced by Cisplatin (1)
- Diabetic nephropathy model in BTBRob/ob mice (2)
- Kidney fibrosis model in rats, induced by unilateral ureteral obstruction (3)
Case study
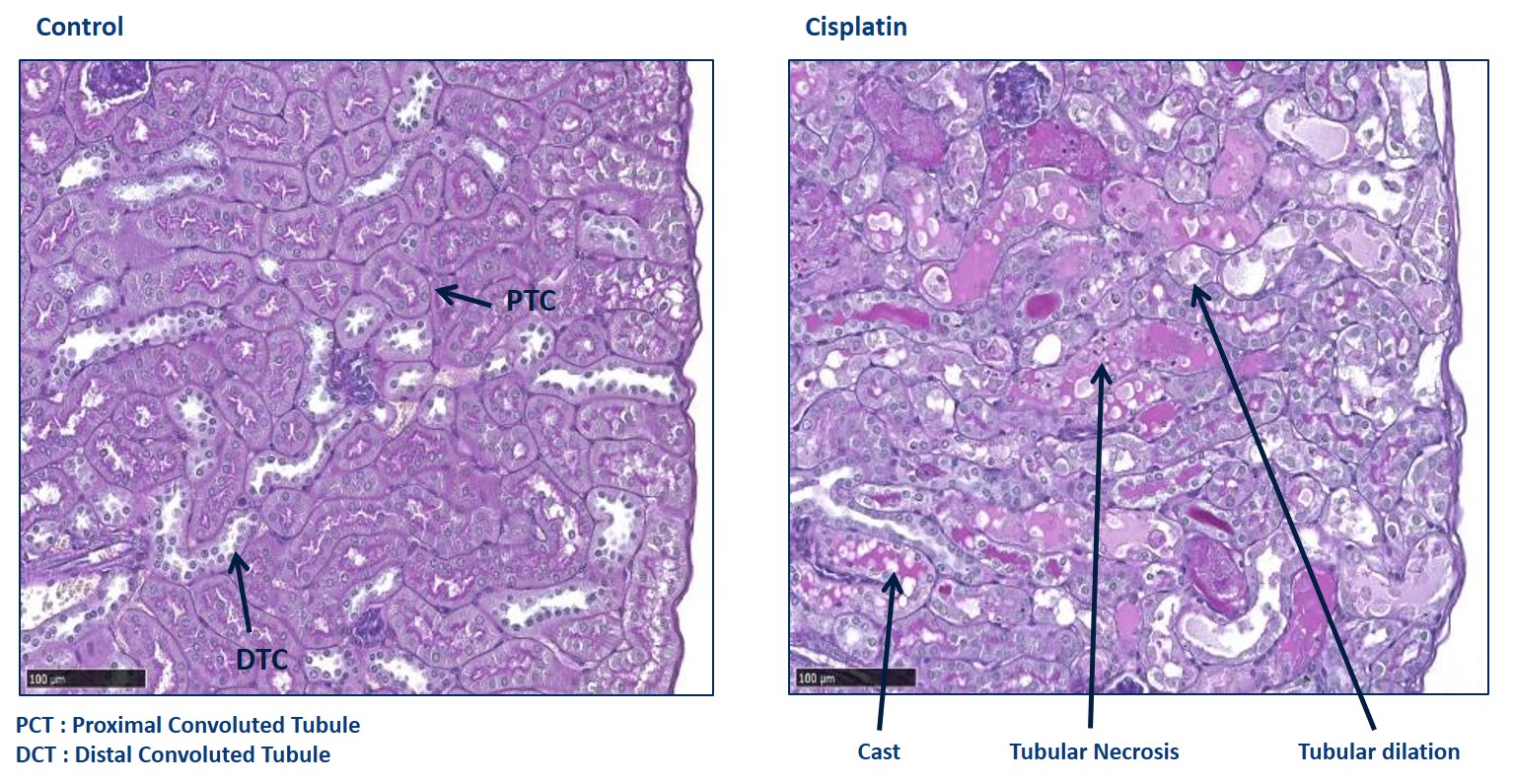
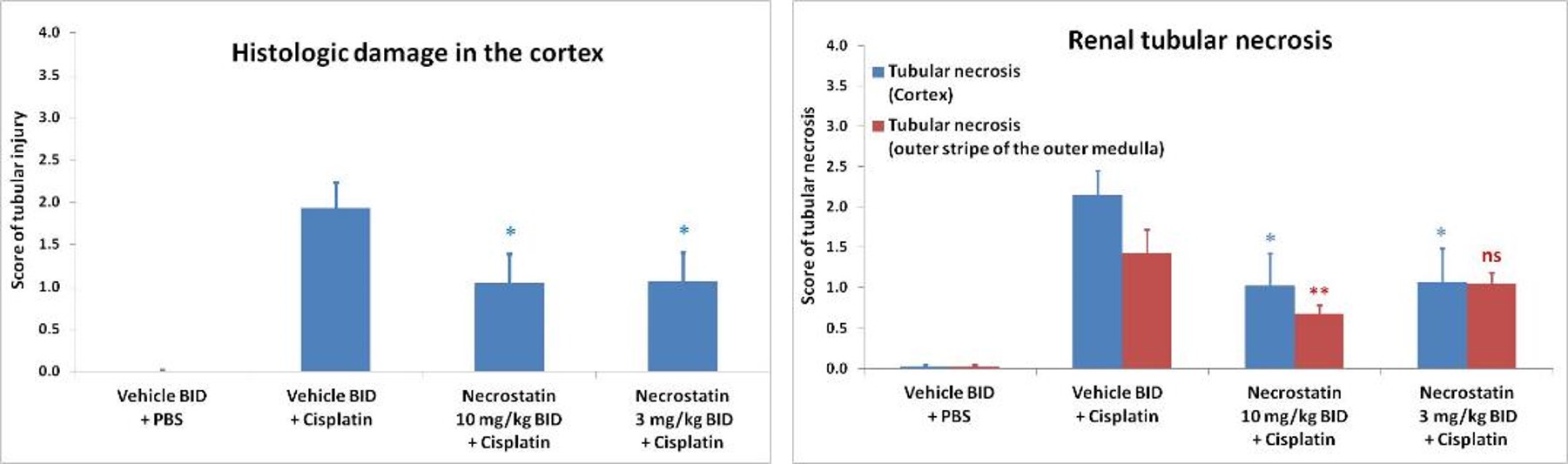
Cisplatin-induced acute kidney injury
While cisplatin induces toxicity on various systems, including gastrotoxicity, myelosuppression, ototoxicity and allergic reactions, the major dose-limiting side effect is nephrotoxicity.
It is estimated that 20% of patients receiving high-dose cisplatin develop severe renal dysfunction and approximately one third of patients experience kidney injury just days following the first treatment.
Typically, serum creatinine and urea rise within 3 days of cisplatin treatment. Necrostatin (RIPK-1 inhibitor) alleviates kidney dysfunction induced by cisplatin.
Also to discover
-
References
(1) Acute kidney injury model in mice, induced by Cisplatin
Luan Z, Wei Y, Huo X, Sun X, Zhang C, Ming W, Luo Z, Du C, Li Y, Xu H, Lu H, Zheng F, Guan Y, Zhang X. Pregnane X receptor (PXR) protects against cisplatin-induced acute kidney injury in mice. Biochim Biophys Acta Mol Basis Dis. 2021 Mar 1;1867(3):165996. doi: 10.1016/j.bbadis.2020.165996. Epub 2020 Oct 27. Erratum in: Biochim Biophys Acta Mol Basis Dis. 2022 Feb 1;1868(2):166305. PMID: 33127475. https://www.sciencedirect.com/science/article/pii/S0925443920303446?via%3Dihub
Chen X, Wei W, Li Y, Huang J, Ci X. Hesperetin relieves cisplatin-induced acute kidney injury by mitigating oxidative stress, inflammation and apoptosis. Chem Biol Interact. 2019 Aug 1;308:269-278. doi: 10.1016/j.cbi.2019.05.040. Epub 2019 May 31. PMID: 31153982. https://www.sciencedirect.com/science/article/abs/pii/S0009279719302819?via%3Dihub
Zhu L, Yuan Y, Yuan L, Li L, Liu F, Liu J, Chen Y, Lu Y, Cheng J. Activation of TFEB-mediated autophagy by trehalose attenuates mitochondrial dysfunction in cisplatin-induced acute kidney injury. Theranostics. 2020 Apr 27;10(13):5829-5844. doi: 10.7150/thno.44051. PMID: 32483422; PMCID: PMC7255003. https://pubmed.ncbi.nlm.nih.gov/32483422/
Lu Q, Wang M, Gui Y, Hou Q, Gu M, Liang Y, Xiao B, Zhao AZ, Dai C. Rheb1 protects against cisplatin-induced tubular cell death and acute kidney injury via maintaining mitochondrial homeostasis. Cell Death Dis. 2020 May 13;11(5):364. doi: 10.1038/s41419-020-2539-4. PMID: 32404875; PMCID: PMC7221100. https://www.nature.com/articles/s41419-020-2539-4
Hamano H, Ikeda Y, Goda M, Fukushima K, Kishi S, Chuma M, Yamashita M, Niimura T, Takechi K, Imanishi M, Zamami Y, Horinouchi Y, Izawa-Ishizawa Y, Miyamoto L, Ishizawa K, Fujino H, Tamaki T, Aihara KI, Tsuchiya K. Diphenhydramine may be a preventive medicine against cisplatin-induced kidney toxicity. Kidney Int. 2021 Apr;99(4):885-899. doi: 10.1016/j.kint.2020.10.041. Epub 2020 Dec 9. PMID: 33307103. : https://www.kidney-international.org/article/S0085-2538(20)31411-3/fulltext
(2) Diabetic nephropathy model in BTBRob/ob mice
- Review:
Alpers CE, Hudkins KL. Mouse models of diabetic nephropathy. Curr Opin Nephrol Hypertens. 2011 May;20(3):278-84. doi: 10.1097/MNH.0b013e3283451901. PMID: 21422926; PMCID: PMC3658822. https://journals.lww.com/co-nephrolhypertens/Abstract/2011/05000/Mouse_models_of_diabetic_nephropathy.12.aspx
- Model characteristics:
Hudkins KL, Pichaiwong W, Wietecha T, Kowalewska J, Banas MC, Spencer MW, Mühlfeld A, Koelling M, Pippin JW, Shankland SJ, Askari B, Rabaglia ME, Keller MP, Attie AD, Alpers CE. BTBR Ob/Ob mutant mice model progressive diabetic nephropathy. J Am Soc Nephrol. 2010 Sep;21(9):1533-42. doi: 10.1681/ASN.2009121290. Epub 2010 Jul 15. PMID: 20634301; PMCID: PMC3013527. https://journals.lww.com/jasn/Abstract/2010/09000/BTBR_Ob_Ob_Mutant_Mice_Model_Progressive_Diabetic.20.aspx
Opazo-Ríos L, Tejera-Muñoz A, Soto Catalan M, Marchant V, Lavoz C, Mas Fontao S, Moreno JA, Fierro Fernandez M, Ramos R, Suarez-Alvarez B, López-Larrea C, Ruiz-Ortega M, Egido J, Rodrigues-Díez RR. Kidney microRNA Expression Pattern in Type 2 Diabetic Nephropathy in BTBR Ob/Ob Mice. Front Pharmacol. 2022 Mar 16;13:778776. doi: 10.3389/fphar.2022.778776. PMID: 35370692; PMCID: PMC8966705. https://www.frontiersin.org/articles/10.3389/fphar.2022.778776/full
Li Y, Hu Q, Li C, Liang K, Xiang Y, Hsiao H, Nguyen TK, Park PK, Egranov SD, Ambati CR, Putluri N, Hawke DH, Han L, Hung MC, Danesh FR, Yang L, Lin C. PTEN-induced partial epithelial-mesenchymal transition drives diabetic kidney disease. J Clin Invest. 2019 Mar 1;129(3):1129-1151. doi: 10.1172/JCI121987. Epub 2019 Feb 11. PMID: 30741721; PMCID: PMC6391108. https://www.jci.org/articles/view/121987
- Testing of compounds:
Sugahara M, Tanaka S, Tanaka T, Saito H, Ishimoto Y, Wakashima T, Ueda M, Fukui K, Shimizu A, Inagi R, Yamauchi T, Kadowaki T, Nangaku M. Prolyl Hydroxylase Domain Inhibitor Protects against Metabolic Disorders and Associated Kidney Disease in Obese Type 2 Diabetic Mice. J Am Soc Nephrol. 2020 Mar;31(3):560-577. doi: 10.1681/ASN.2019060582. Epub 2020 Jan 29. PMID: 31996409; PMCID: PMC7062217. https://journals.lww.com/jasn/Abstract/2020/03000/Prolyl_Hydroxylase_Domain_Inhibitor_Protects.12.aspx
Locatelli M, Zoja C, Conti S, Cerullo D, Corna D, Rottoli D, Zanchi C, Tomasoni S, Remuzzi G, Benigni A. Empagliflozin protects glomerular endothelial cell architecture in experimental diabetes through the VEGF-A/caveolin-1/PV-1 signaling pathway. J Pathol. 2022 Apr;256(4):468-479. doi: 10.1002/path.5862. Epub 2022 Feb 23. PMID: 35000230. https://onlinelibrary.wiley.com/doi/10.1002/path.5862
(3) Kidney fibrosis model in rats, induced by unilateral ureteral obstruction
- Compound efficacy:
Tingskov SJ, Jensen MS, Pedersen CT, de Araujo IBBA, Mutsaers HAM, Nørregaard R. Tamoxifen attenuates renal fibrosis in human kidney slices and rats subjected to unilateral ureteral obstruction. Biomed Pharmacother. 2021 Jan;133:111003. doi: 10.1016/j.biopha.2020.111003. Epub 2020 Nov 20. PMID: 33227702. https://www.sciencedirect.com/science/article/pii/S0753332220311951?via%3Dihub
Mizutani A, Endo A, Saito M, Hara T, Nakagawa M, Sakuraya K, Murano Y, Nishizaki N, Hirano D, Fujinaga S, Ohtomo Y, Shimizu T. Hydrogen-rich water reduced oxidative stress and renal fibrosis in rats with unilateral ureteral obstruction. Pediatr Res. 2022 Jun;91(7):1695-1702. doi: 10.1038/s41390-021-01648-7. Epub 2021 Aug 7. PMID: 34365467 https://www.nature.com/articles/s41390-021-01648-7
Case study:
Cisplatin-induced acute kidney injury: Same references as above.